UNDERSTANDING ‘LONG COVID’
ECU partnering with Dartmouth to study, treat chronic COVID-19
A team from ECU’s Brody School of Medicine is collaborating with health care providers from Geisel School of Medicine at Dartmouth to understand the extended effects of COVID-19, and to provide resources and guidance to patients whose symptoms persist beyond the usual duration.
It’s known as “post-acute COVID-19 syndrome,” “long COVID,” “chronic COVID” and sometimes “long-haul COVID.” The CDC refers to the range of aftereffects experienced by some who have had COVID-19 as “post-COVID conditions.”
“By definition, it is persistent symptoms beyond four weeks of onset of symptoms,” said Dr. Paul Bolin Jr., chair of internal medicine at the Brody School of Medicine, who is among those leading the ECU and Vidant Health teams treating COVID-19 infected patients and working to vaccinate community members across the region.
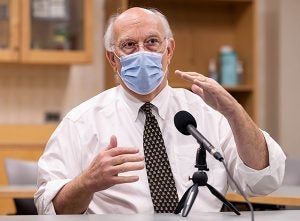
Dr. Paul Bolin Jr. discusses the latest information about COVID-19 during a recording for the Talk Like a Pirate Podcast.
“It spans the whole spectrum — there’s people who have had nothing more than loss of taste to people who were in the ICU for a month,” Bolin added. “We’re seeing persistence of fatigue, shortness of breath, unusual pain syndromes. Some people with loss of smell and taste for prolonged periods of time, a lack of mental clarity — cognitive fog, if you will. There have been studies that have documented significant decreases in cognition after COVID.”
Much remains unknown about COVID-19, including its long-term effects on the body and the brain, and why some patients fare worse than others when they become infected by it.
This is what brought teams of health care providers and researchers from ECU and Dartmouth together — to better understand these issues and find solutions for those struggling to fully recover.
As Bolin and his team have met with chronic COVID patients in person, they also have a standing virtual meeting with their Dartmouth collaborators so that the teams can learn from one another and adjust their strategies.
“I think the benefit to collaborating is that we have different demographics. We both have rural populations, but I think we have a very rural, largely Caucasian population in New Hampshire and Vermont,” said Dr. Jeffrey Parsonnet, professor of medicine at the Geisel School of Medicine. “So there are demographic differences in the populations that inform the understanding of this syndrome. There are geographic differences and there’s the reality that as you get more numbers you get additional information. Also, having researchers with different histories, different perspectives, different backgrounds help develop a research proposal.”
“We saw something like this after the 1918 pandemic. It was noted that many people after the 1918 flu actually ended up with Parkinson’s,” he said. “The (chronic COVID) research involves cataloging all of these symptoms.”
Bolin said there is currently no treatment for chronic COVID, because physicians and researchers do not know what it is.
“We’re trying to pick apart those pieces. It is probably several things,” said Bolin, adding that for patients who were sick enough to be admitted to the ICU, Post-ICU syndrome can cause extreme fatigue and muscle wasting, and can be one of the contributing factors preventing people from recovering fully. “We do know that with COVID there’s an entry portal between the olfactory bulbs that lie just above the nasal cavity — this is why people lose their sense of smell. There’s now documentation that the virus actually enters the CNS (central nervous system) — the brain. So, there probably are some, at least, of these folks who have had some type of direct CNS insult.
“A lot of people have had clotting issues — sometimes that’s in the brain, sometimes it’s in the chest, sometimes that’s in their legs and they’re weak in their legs. It’s just an amazing array of symptoms.”
Some chronic COVID patients who have recovered from acute COVID-19 have been found to have immune systems that are malfunctioning, creating autoantibodies that can target an individual’s otherwise healthy proteins. This could be related to the patients’ ongoing symptoms, Bolin said.
“It may be that there will be a trial — I hope — where we would give immunosuppressive agents to block those antibodies,” he said. “It may be those antibodies are driving those symptoms. So this chronic COVID may end up being an autoimmune disease.”
Although there currently are not approved treatments for long COVID, Bolin’s team has been able to provide patients with referrals to specialist care — commonly rehabilitation, pulmonary or neurological — and work with their current health care providers to assess and revise their medications as needed. Bolin also emphasized that by seeing these patients and documenting their cases, their team then has a way to contact them when a promising treatment emerges.
Many patients, though, find some relief in hearing that they’re not imagining their symptoms, that they’re not alone in experiencing these ongoing issues and that teams like Bolin’s are working to understand them and find solutions.
“Nobody comes to this COVID clinic without crying,” Bolin said. “The reason they cry is because it’s the first time somebody has told them this is real. This is the most amazing thing about this, to me, is that these people have lived with this. I think a lot of people — trying to be encouraging — have told people, ‘Oh you’re fine, just keep going’— and they don’t feel fine. So, you get this label of you’re faking it, or you just think you are sick.
“It’s amazing when I tell people this is real, invariably they’ll burst out crying because they’ve been carrying that emotional burden that it’s their fault, so to speak.”
For more information about the long COVID clinics or to make an appointment, contact Caryl Holoman at 252-744-2570 or holomanc@ecu.edu.
