COVID-19 Q&A
ECU’s medical and scientific experts answer some of the most pressing COVID-19 questions
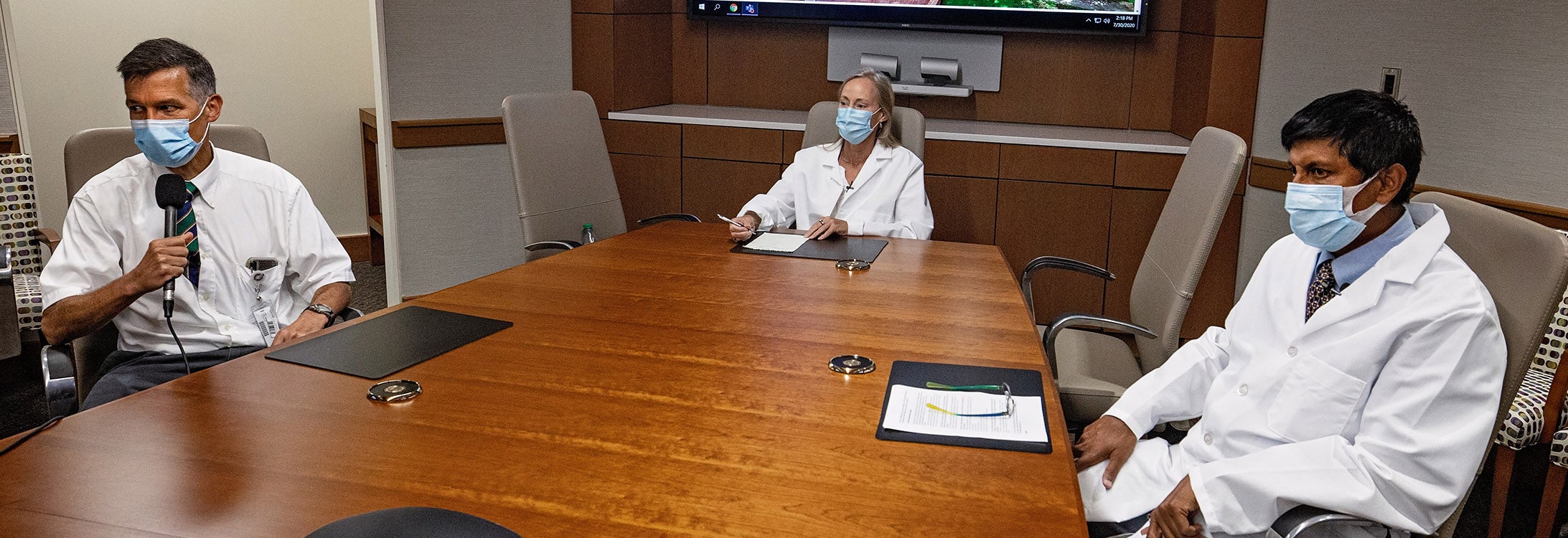
As we entered August still in the midst of the COVID-19 pandemic, we spoke with three of our faculty experts from ECU’s Brody School of Medicine to get answers to some of today’s most pressing questions and discuss some of the theories we’ve seen floating around on social media.
Dr. Shaw Akula is an associate professor in the Department of Microbiology and Immunology. A virologist, he primarily focuses on herpes viruses associated with AIDS, but recently has begun working with Dr. Paul Cook on understanding the molecular signature of the novel coronavirus and COVID-19.
Dr. Paul Cook is the chief of the Division of Infectious Diseases at the Brody School of Medicine as well as a clinician for ECU Physicians Medical Practice and Vidant Medical Center. Among his other work and his research with Dr. Akula, Cook is directing a clinical trial that aims to prevent COVID-19 from causing an often fatal type of lung damage in patients. He is also preparing to begin a new outpatient trial of a monoclonal antibody to the spike protein of SARS-CoV-2.
Dr. Rachel Roper is an associate professor in the Department of Microbiology and Immunology. Roper worked on the original SARS coronavirus in 2003 and was part of the group that first did the genome sequence and analysis on that virus. Roper oversaw two vaccine trials in mice and ferrets in the early 2000s. She is currently working on diagnostics and a COVID-19 vaccine while setting up a biosafety level 3 high-containment lab for growing the virus at ECU.
Visit YouTube for the closed-captioned version of this video.
(Video and Podcasts by Rich Klindworth)
READ OR LISTEN
Continue scrolling to read each section or use the jump links below to visit any of the three sections. Rather listen? Our special three-part Talk Like a Pirate podcast is available at the start of each section.
VACCINE PROGRESS AND TREATMENTS FOR COVID-19
Q: We are now five or six months into the COVID-19 crisis in the United States and even longer when you look at its origins. We were told from the beginning that a vaccine was a year/year-and-a-half away. So, we’re either a third or halfway to that initial approximated timeline. From everything you know, how much closer are we to a vaccine?

Dr. Rachel Roper, shown working on a project prior to COVID-19, is currently working on diagnostics and a COVID-19 vaccine while setting up a biosafety level 3 high-containment lab for growing the virus at ECU.
Dr. Rachel Roper (RR): We have 100 vaccines in trials right now, and the question is do we have enough data that they’re safe and do we have enough data that they’re effective. For any vaccine to be approved, the FDA has to have data that shows that it’s safe and efficacious. Right now, we have data from several vaccines that look like they’re safe to use in humans — we haven’t seen any concerns. They’ve been able to demonstrate immune responses — antibodies to the proteins and even neutralizing antibodies that are able to neutralize the virus, but we don’t actually have efficacy in humans. There are some trials in animals that have shown protective efficacy in primates.
Dr. Shaw Akula (SA): As of now, most of these are projected dates. There are several companies that are making the vaccine — the giants like Johnson & Johnson, Merck, Pfizer — their projected dates are early- to mid- 2021. The Moderna vaccine is supposed to come as early as January 2021. All of these are projected dates. We don’t know how effective it will be or are they going to be released at the time projected. I might add that it will definitely make stocks go up, but I don’t know whether it’ll do the job effectively as of now.
Dr. Paul Cook (PC): These vaccine trials historically have taken years. I don’t think we can wait years, but it’s certainly going to be longer than months.
Q: Many people are concerned about society “rushing” for a vaccine and/or treatment. Therefore, they say they are hesitant to get a vaccine when it is approved. Should they be hesitant to get a vaccine when it’s approved?
RR: We won’t have as much safety data on this vaccine as the ones we’ve been using for many years, but there will be safety data that looks like it is safe in humans. Every medical intervention is a balance between risk and benefit, so you have to weigh the risk of the vaccine versus risk of not getting the vaccine and getting COVID. So, with 150,000 dead Americans, I think I’m going to get the vaccine.
SA: I do respect when some of them are skeptical. We have to respect that. As Dr. Cook mentioned, under normal circumstances it always takes many years to develop a vaccine so it’s normal for some people to be skeptical.
RR: There could be some rare side effects that you don’t see when you vaccinate 1,000 people but you do see when you vaccinate a million people. We have 330 million in America, so we could end up seeing some adverse events later. In the past, there have been problems with certain vaccines, so it may take a few years to get it right.
Q: Do you foresee a potential vaccine for COVID being a one-time vaccine more like polio or smallpox or do you imagine it could be similar to the flu vaccine that people should get annually?
RR: Coronaviruses have one large piece of genome. They’re very different from influenza viruses, which have eight different pieces or segments of genome. So they naturally, in the wild, exchange these genome pieces regularly, which is why we have a new — or several new — influenza viruses every year and why you have to make a new vaccine every year. SARS coronavirus is one large piece so it will not do the switching of genetic pieces as easily as influenza does. It should be more like measles, mumps, rubella, where you can make one vaccine that lasts for years. But it will mutate over time and if we’re only hitting a small target in the vaccine, it’s more likely to mutate away from that vaccine protection than if we’re using an attenuated virus vaccine like we do for measles, mumps, rubella, polio.
SA: I agree with Dr. Roper, but I feel that it will definitely not be on the lines of a polio (vaccine), where you get it once and you’re done for a lifetime. In this case there are several strains out there. Of the multiple strains, they’ve grouped them into four groups and three subgroups, but it’s evolving… There are so many strains, so it will definitely not be like polio — one shot — but there is more of a chance to be multiple rounds of vaccinations. That is my thought.
RR: The polio virus vaccine — the main one used — is an attenuated virus vaccine. That means the immune response is to pretty much the entire virus. A lot of the vaccines that are being made right now for the coronavirus are focused on spike — one little piece of the whole genome, so it’s a much smaller target so there’s going to need to be at least vaccinations and boosts — maybe even three vaccinations before you get good efficacy on it because none of the vaccines we have right now are targeting large pieces of the whole SARS Coronavirus genome for COVID.
Q: Have we ever had a successful vaccine for coronavirus?
RR: There’s a pig coronavirus vaccine that is used. There’s another one used for dogs. So, there have been some used in veterinary practices because we never really tried to make a human coronavirus vaccine because we never had a major human pathogen that was a coronavirus. We just had coronaviruses that would cause the cold until we had the first SARS in 2003 and that was controlled with public health methods by isolation and quarantine. So, we never really got to the human vaccine trial because it disappeared from the world.
Q: Dr. Roper, you’re working on a vaccine right now?
RR: I’ve got funding from the North Carolina Biotechnology Center and also an industrial partner to work on making vaccines for COVID using different SARS coronavirus genes cloned into ECU’s patented/my improved vaccine vector platform, which I hope will give better efficacy than just using the spike (protein) that many of the companies are doing now. Especially for elderly people, the vaccine just to spike might work for younger people, but older people have a weakened immune response and it might be better to have more targets for their immune response to be able to react to. That’s what might increase vaccine efficacy, so that’s one of the things that we’re looking at.
Q: What’s it like to be working on a vaccine right now?
RR: Well I wish we could go faster (laughs). There’s a lot of paperwork, setting up the labs. There’s a lot to do. I had all my original projects before coronavirus hit. So now I have twice the amount work and a lot of the other things are getting left behind. But this (coronavirus vaccine) is the priority and we have to do it.
Q: There’s a lot of discussion about which treatments are the most promising right now. In your opinion, what are some of the more promising treatments for COVID patients as we understand them right now?
PC: There’s no FDA-approved treatment for COVID. There are some investigational drugs. There’s the drug remdesivir that’s not FDA approved, but that’s been given this emergency use authorization by the FDA. The data suggests that it does help in certain situations. It’s helpful, but it’s not like taking penicillin for strep throat — it doesn’t work that well. We’ve got some other treatments which are supportive including dexamethasone which has received a lot of press recently for persons who are severely ill and, particularly those on mechanical ventilation or requiring high supplemental oxygen. We’re working on this monoclonal antibody to this substance angiopoetin-2. We’ll see how that works out — this is a randomized, double-blind trial, so we won’t know the data until the study’s completed which is likely to take a couple more months.
Q from RR: There’s also an interferon beta inhalant. Have you heard about that?
PC: Yes, I have heard about it. We don’t have access to that here, but I think given what we know about what the virus does to the innate immune system, it seems like a pretty good idea.
Q from RR: Was it Paul Bolin that was working on the convalescent serum?
PC: The convalescent serum is sort of fading, and what I mean by that is the supply nationally has gone way down. That’s one of the reasons Dr. Bolin asked if we could be a site for this monoclonal antibody to the spike protein. He used that as sort of the replacement for the convalescent plasma and I think it’s probably a big improvement over convalescent plasma.
These different plasmas from different donors — we don’t know what the titers of the neutralizing antibodies are from one donor to the next, whereas with a monoclonal antibody we know pretty much exactly what these persons are getting.
SAFETY, MASKS AND REOPENING
Reader-submitted question: How often should someone get tested, and what type of test should people get?
RR: The only test that actually detects active infections is the polymerase chain reaction (PCR) that detects the viral genome. That’s usually done with a nasopharyngeal swab, although sometimes they’re doing it with throat swabs. Actually, we’re working on developing it for saliva, which has a lot of advantages: you don’t need a swab and you don’t need a health care professional to take the sample. And, it’s a lot easier to get a saliva sample than a nasopharyngeal swab.
The polymerase chain reaction (PCR) test should be used for diagnostics. You cannot use the antibody test for diagnostics because people don’t make antibodies for sometimes weeks after the virus infection. There’s another kind of test coming on which is the antigen test. So, instead of detecting the viral genome you’re detecting the viral proteins. The problem with those is they’re not very sensitive — so if you test positive, you can trust the result and you’ve really got it. If you test negative, you don’t know and you should get a nasopharyngeal swab.
If you get exposed one day and get tested the next day, I think you’re going to test negative because it’s during the incubation period. It could be a week before you develop symptoms and the virus has to grow to high enough levels in the tissues to be detectable by the PCR test. You will be negative one day and positive the next, we just don’t know exactly when that will be and it probably depends on the dose of the virus that you got when you got infected. So, it’s complicated.
SA: I would say why fix it if it’s not broken? Unless you’re showing some small symptoms, why go and get tested? That’s my opinion.
RR: We know a lot of people who are asymptomatic can spread the virus. Some estimates I’ve seen suggest up to 50% of infections are spread by people that are completely asymptomatic. That’s one of the reasons that everybody needs to wear a mask — you could go in a store or be near other people and you could be exhaling virus all over the place and infecting other people when you don’t even know it. The mask needs to cover both the mouth and nose to help protect you and other people from the virus.
There has been concern from people on social media that if you wear a mask it’s going to make you sick — that it’s going to hold the virus in. But if you already have the virus you can’t catch it from yourself.
PC: Yeah, you can’t catch a disease from yourself.
Q: What is being done/what can be done at ECU to keep people safe?
RR: There are lots of signs up that everyone should be wearing masks, washing their hands, keep physical distancing. The Brody School of Medicine has a whole list and east campus does as well as to what you’re supposed to do. Anyone who has any respiratory symptoms should not come in and should contact health care professionals.
Q: We’re coming into allergy season and we’re coming into flu season. So, if someone has the sniffles, should they stay away and get tested? What’s the line to know what to do?
PC: Well the screening symptoms are not perfect. The ones that are most specific are cough, fever and loss of sense of smell. So if somebody has those symptoms, it’s fairly likely that it’s SARS-CoV-2. If they’ve got cough and fever and it’s November or December, it easily could be flu. If they’ve got the sniffles, it could be the common cold or another of the coronaviruses that are not deadly. We can’t test everybody who has the sniffles.
RR: So, everybody should get their flu vaccine this year. You don’t want to end up having flu and having to go into the emergency room which is already going to be busy. You don’t want to go in with flu and come out with COVID.
Q: Are we able to have students go back to schools and colleges safely?
RR: Well there’s some risk just walking around the United States, and not just from COVID, but from other things as well. So, it’s a matter of how risky it is, and everybody can do things to protect themselves — keep distance, wash your hands, wear a mask, don’t touch your face when you’re out touching other things. It’s a matter of risk and the benefits of getting an education and having social interaction. It’s a difficult choice.
PC: Everything has its risks. Education is risky, and it’s a lot more risky now than it was last year.
Q: At first, we were told masks were a waste of money. Now it’s mandatory in many places that you have to wear them. What went into this change of attitude?
PC: One of the benefits of the pandemic is that a lot of people have collaborated, and we have a lot more information now than we did in the first of March or in February. I remember giving a lecture March 2 on east campus on the risk of COVID. At that time, North Carolina had zero cases and I remember telling people not to wear masks in public because that was what the recommendation was. Since that time, we’ve learned a lot more about how this virus is spread, and it’s spread a lot more readily than influenza. Studies that have been done have shown that masks are very effective in preventing transmission. They’re not 100%, but very few things are. Masks work if people use them appropriately.
Q: When you’re not in the hospital or research lab, what type of PPE are you using for everyday activities like going to the grocery store? What is the best type of mask for the average person to wear?
PC: I think there’s some recent data that layers of masks are more effective. It sort of makes sense. I used to live in the north and layers protect you from the cold and layers also apparently are also more effective than a single layer of a mask. So I think we’ll probably see more of these multilayered masks.
Q: What’s the safest way to reopen schools?
SA: Virtually. Virtual or online is the best way, but is it doable for everyone? Every family is different. Virtual is less risky. When you increase the number of students in a place or people in a place, the chances (of infection spread) increase.
PC: Yeah, I don’t think there’s one-size-fits-all. Opening schools in Florida or Texas or Arizona would be a disaster right now.
Q: But North Carolina?
PC: North Carolina is not nearly as bad as Texas or Florida, but it’s a lot worse than Maine. The virtual makes the most sense from the standpoint of safety. The problem is in our area we’ve got a discrepancy as far as income and a lot of people aren’t going to be able to do virtual learning. They just don’t have the means to do that. The other issue is that some people respond to virtual learning a lot better than others.
Q: Is it important for people who have had COVID to continue doing things like wearing a mask, staying 6 feet apart, etc.? Why?
SA: Absolutely, they should wear their masks.
PC: I agree, and there are several reasons it would be bad for them not to wear the mask. 1. It sends the wrong signal to other people. 2. There are other infections that can be transmitted through the respiratory route as well and some of them act a lot like COVID, like influenza for example.
Q: Should we travel to other states and visit our loved ones or have them come here?
SA: If you love them, don’t travel. Wait until things settle down, and then you can show your love.
RR: I’m not traveling anywhere in the near future. We’ve had family weddings cancelled. I would not get on a plane. If you’re driving in your car — maybe. People are getting RVs and staying in RVs so they’re not staying with family members. But the more contact you have the more you can spread it and catch it.
PC: I was just on a plane yesterday — two planes.
RR: How full were they and how masked were people?
PC: Well, masks were required. They said that if you do not wear a mask you will not be put on a plane now or in the future.
Q: Is it safe to eat at a restaurant? Does eating outdoors really make you that much safer?
RR: I’m much more comfortable eating outside at a restaurant. I really don’t want to eat inside at a restaurant right now. It doesn’t seem that safe. Some restaurants are being really good and really careful about cleaning things and keeping people distanced and wearing masks, but any place indoor for a long period of time — especially because you have to take your mask off to eat, you’re exposing yourself and potentially exposing others.
Q: Are there any activities that have been allowed to “resume” that maybe should not have resumed?
RR: I agree with public health officials in that gyms and bars are more dangerous than other places. Gyms — you’re breathing heavy. Especially if you have a lot of people in there, gyms seem less safe to me. At bars you have people drinking and people tend to lose their inhibitions, people are speaking loudly frequently in bars and that makes it more dangerous, too. Singing in church is also a dangerous thing to do — singing outside is better than singing inside.
Q: Is there any chance we can hug our loved ones anytime soon?
RR: If you wear a mask and don’t breathe on each other. If you look the other way, I suppose you could get away with it, but it’s a risky thing to be close to someone, especially if you’re not masked.
SA: Especially if they’re elderly, they’re in the high-risk category. So you can be with them but not get too close. It’s better to take a lot of precautions.
RR: Another thing is that obesity is a significant risk factor. I believe the statistics say 40 percent of Americans are obese, so half of America is in the high-risk group. So we need to remember that… It’s not just older people that have to worry about it. More and more we’ve got younger people being hospitalized.
MYTHBUSTING AND UNDERSTANDING THE NEWS
Q: Can people who have had COVID already get it again?
RR: Maybe. We’re not sure. My guess is that it wouldn’t be as bad if they do get it (again) and they probably would be protected, but we don’t know for sure at this point.
Q: Did COVID originate in a lab in China?
RR: No! I’ve looked at the genome sequence. It looks like the other coronaviruses that are circulating. It looks completely natural, there’s no unusual sequence in there at all. It’s very similar to the first SARS coronavirus that broke out in 2003. In the receptor binding domain there are six amino acid changes that no one could have predicted would work, so I don’t think anybody could have designed this. And if they did, how would they have tested it? It’s just implausible. There’s no evidence at all (that it was created in a lab) and the scientific consensus is that it’s completely natural.
Q: With it being natural, could it have leaked out of a lab in which it was being studied?
RR: Probably not. If it’s already in the wild, why would we think it would come out of a biosafety level 3 lab where everyone’s very careful? They know that people that do spelunking in the caves where the bats are — those people already have antibodies to these viruses. There’s a whole bunch of them already circulating over in Asia. So you don’t have to make it in a lab or get it from a lab — it’s already out there in nature, and it’s jumped into the human population now twice significantly.
Q: So do we know that it came from bats?
RR: The evidence is very good that it’s from bats because so many of the bat coronaviruses are so closely related. North American bats don’t have coronavirus — there’s never been any outbreak like that in North America, so don’t kill your bats — they’re good in North America.
Q: What are the data points that people should be looking at to evaluate how we’re doing in managing this disease? Infection rates? Death rates? Something else? Where’s the best place to find this information?
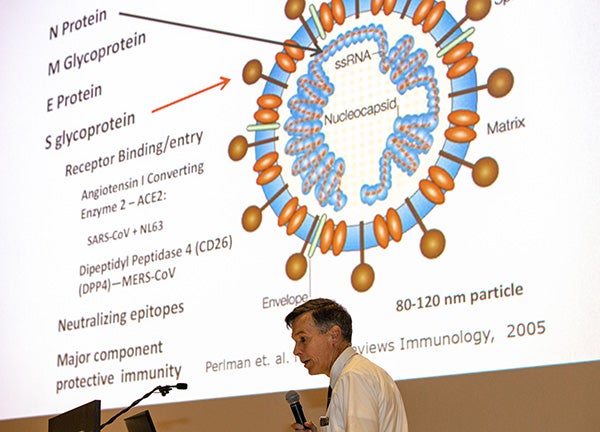
Dr. Paul Cook, Chief of the Division of Infectious Disease at the Brody School of Medicine gives a lecture about COVID-19 at ECU’s Black Box Theater in early March, prior to when North Carolina had any known cases of the virus.
PC: The CDC site, the department of health and human services, both at the national level and the state level are very reliable sources.
RR: And the Johns Hopkins website. There’s also the World-o-Meter, which is pretty good, but Hopkins is the most reliable one that’s generally followed and believed. You want to look at infections, hospitalizations and deaths. I would look at all three of those. Deaths are going down as we learn how to treat patients better, and infection rates can go up if you do more testing, but hospitalizations, in my opinion, might be the best, most stable one to look at because I don’t think that criteria is changing that much for deciding who gets admitted to the hospital.
PC: The hospitalizations in North Carolina have gone up in the past month. The number of deaths has actually gone up in the last month as well. People have made a lot of comments about the death rates going down, and in general they have but with the increases in the number of hospitalizations, there has been an increase in the number of deaths.
RR: Because deaths will lag admission by weeks.
PC: They typically do, and in fact the patients that we’ve seen in this study that have died, they’ve usually died after two or three weeks in the hospital and not usually within a couple of days after being admitted.
Q: Many people are dismissing the increasing numbers, blaming it on an increase in testing. Is there any truth to that?
RR: Just a little bit. The more you test, the more you’re going to find. But as Dr. Cook said, we’ve got increasing hospitalizations and now increasing deaths. A lot of people thought because the hospitalizations were going up and deaths were going down that some people were claiming that it was becoming less virulent, less pathogenic. But it was just the lag time and physicians are treating it more effectively now. There have been things that have been learned to take care of patients better.
Q: Some people are still comparing COVID-19 to the seasonal flu and wondering why we’re doing things like having people who aren’t exhibiting symptoms get tested. What’s your response?
RR: We have 150,000 dead Americans in just a few months. In a bad year, flu could kill 60,000 all year, and COVID already has 150,000 deaths in just a few months, and that’s with closing down the economy, with masks, with social distancing. So COVID is much worse than influenza and should not be confused with flu.
PC: It’s not the flu. It’s much worse than the flu. The mortality rate is much worse than the flu, the transmissibility of the virus is much worse than influenza. This is a much worse viral disease than the flu… This country has done a pretty lousy job of testing. If you don’t test you won’t find infections.
RR: If you actually look at the number of cases that are known and the deaths, it comes out to about a 10 percent fatality rate, but that’s not real because a lot of people got infected and aren’t counted in the number of infected people. So that makes the death rate look too high.
Q: Some are saying that people are dying from heart attacks or other causes unrelated to COVID, but being counted among COVID deaths. Is there any truth to that?
PC: Certain infections, such as influenza, put you at a higher risk of having a heart attack. A lot of these conditions that we don’t usually associate with infection such as a myocardial infarction or a heart attack actually can be precipitated by infectious processes including influenza and including COVID-19. So, the inflammatory response is very closely associated with thrombogenesis or clot forming and that’s how we get heart attacks and strokes and things like that. So, to say somebody died of a heart attack and it wasn’t associated with COVID, it’s very simplistic and downright wrong.
Q: Are there any other concerning trends that you’re hearing about from news or social media that you think would be good to clarify?
RR: One of the things that I’ve had people talking about recently is a lot more appreciation of how it’s spread through the air and how important masks are. That’s causing a lot of people I know to think it’s not transmitted by touch. People should not forget to wash their hands and use hand sanitizer, and avoid touching their face. It’s still going to be transmissible that way.
Q: Why do you think it is that COVID-19 has become so polarizing that you don’t know who to believe?
PC: Well, it’s been politicized. COVID-19 is not a republican and it’s not a democrat. It’s not an independent. It’s COVID-19. It doesn’t vote. It’s an equal opportunity infectious agent. It has nothing to do with politics, and politics have taken control. People that don’t wear masks are making a political statement, in my mind, and that’s not a good idea.
RR: But we really do know who to trust — the U.S. government, Centers for Disease Control, White House officials are giving good information out, health and human services is giving reliable information. Some people send me blogs from some guy or some woman that they’ve never heard of, and they’ll believe those instead of trusting reliable sources.
Q: Is there any fear that COVID-19 will affect an internal organ like your heart and stay in your system and hurt you down the line.
PC: We think about its effects on the lungs. Probably more accurate is this causes endotheliitis. If that’s in the lungs, you get this acute respiratory distress syndrome (ARDS). If it’s in the heart and you get clotting there, you can get either myocardial infarction, heart attack or you can get myocarditis. That’s not unique to COVID-19 — influenza can do the same thing. These are rare, but recognized complications of these infections. Just a month and a half ago, a 27-year-old otherwise healthy but obese white male was admitted to a hospital with some abdominal pain and it turns out he was having a heart attack. Within 24 hours he was dead. What he died of is myocarditis related to COVID-19. He had no other risk factors. His 26-year-old wife is pregnant with their only child. So, if young people think this can’t kill them, they’re wrong. This is a deadly disease that needs to be taken seriously.
RR: There’s more and more reports coming out of patients reporting continuing symptoms for months afterwards. There may be scarring in the lungs that may be permanent as well, so they may have decreased lung function permanently.
SA: It’s too early to know because we’re only about six months in. With time we’ll know more about whether a latent infection can sit in there and cause infection later.
Q: What are the craziest COVID-19 myths that you’ve heard so far?
RR: Aliens. Isn’t there someone saying something about an alien genome? Oh and the 5G! People got confused between computer viruses and biological viruses and thought that a 5G computer network was causing this.