BACTERIAL BANTER
Brody researchers awarded grant to study how pathogens ‘talk’
Two researchers at the Brody School of Medicine have received a grant from the National Institutes of Health to continue the work they began years ago on one of the world’s most common bacterial pathogens.
Everett “Eb” Pesci and Jim Coleman, professors in the Department of Microbiology and Immunology, were recently awarded a four-year grant totaling $1,475,851 to continue studying the bacterium Pseudomonas aeruginosa, which Pesci said is “everywhere.”
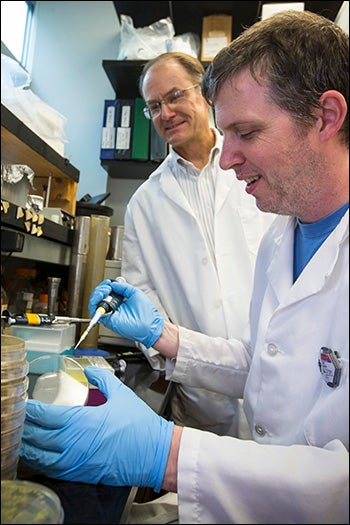
Graduate student John Farrow isolates colonies of Pseudomonas Aeruginosa while Pesci looks on.
“It’s commonly found on flowers, vegetables and things like that,” he said. “We eat it all the time, but healthy bodies can fight it off.” Pesci said the bug is opportunistic, meaning it infects people whose immune systems are compromised in some way due to illness.
Pseudomonas aeruginosa is responsible for about 10 percent of all hospital-acquired infections, causing ailments such as pneumonia, and urinary tract and surgical wound infections.
It also infects most cystic fibrosis patients at a very early age and causes a chronic pneumonia that is very difficult to cure. Cystic fibrosis is a genetic disease in which patients produce an unusually thick, sticky mucus that clogs their lungs and leads to life-threatening lung infections.
“Pseudomonas infections are difficult to treat because there aren’t a lot of antibiotics that will kill these organisms,” said Pesci. “But scientists are starting to believe that maybe you don’t need to kill them – you just need to interfere with their communication.”
Pesci said he and Coleman are studying the communication system that pathogens use to control their virulence, or ability to cause disease. In particular, they will focus on one chemical intracellular communication signal they discovered when they began collaborating in 1998. They call it the Pseudomonas Quinolone Signal, or PQS.
“Basically the bacteria use this signal to talk to each other and to tell the whole bacterial population to delay expressing virulence factors until enough bacteria are present to overcome the host’s immune response,” Pesci said. “Once enough of them are gathered and the environment is ideal, the bacteria will send the signal out that says, ‘now’s the time to turn it on and get the job done.’”
“If we can figure out how to mess with those signals so they can’t talk to each other, it could lay some groundwork for the development of a therapeutic treatment for Pseudomonas infections,” Coleman said. “That could have a great impact for cystic fibrosis patients, for patients who are on respirators and for burn patients.”