Carotid artery angioplasty offers patients alternative to surgery
GREENVILLE, N.C. (Dec. 20, 2001) — Specialists at Pitt County Memorial Hospital are using a minimally invasive procedure to treat selected cases of carotid artery disease. The disease, in which the carotid artery in the neck becomes clogged, is normally treated with an invasive surgical procedure in which the vessel is opened and cleared.
Vascular surgeons from the Brody School of Medicine at East Carolina University have joined vascular-interventional radiologists from Eastern Radiologists in performing angioplasty and stent placement to treat the stenosis, or narrowing of the artery.
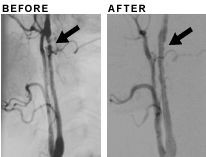
The image on the left shows the narrowing in the carotid artery of a 54-year-old woman. The image on the right after angioplasty shows the artery opened and blood flowing normally. Images courtesy of Dr. Frank Parker.
The most recent case completed using minimally invasive carotid artery angioplasty was performed Nov. 27 at PCMH on a woman from Edenton. Carotid angioplasty uses a balloon catheter to treat the narrowing of the carotid artery as a substitute for the surgical approach of carotid endarterectomy.
This surgical approach is still the main course of treatment for carotid artery disease, though less invasive carotid angioplasty and stenting is being performed on selected patients with good results, according to Dr. Karl Chiang, an interventional radiologist with Eastern Radiologists. Chiang did a similar case in May.
Dr. Frank Parker of the medical school’s section of vascular surgery said the 54-year-old woman was a good candidate for carotid angioplasty because of the type and location of the blockage in her carotid artery. The carotid artery is a large vessel supplying blood to the head, neck and brain and can become blocked by fatty deposits or blood clots.
“She had a rare form of narrowing in the carotid artery high in her neck going into her head. It was above where traditional surgery can reach safely,” he said. Parker, assistant professor of surgery, performed the procedure along with Dr. Steven Powell, professor of surgery and section chief for vascular surgery.
During the procedure, a balloon attached to a catheter – a long tube – is inserted into an artery in the groin and threaded up to the narrowed carotid artery in the neck. Once the catheter is in place, a balloon on the end of the catheter is inflated, pushing the fatty deposits toward the sides of the artery. In most cases a metal stent, which is a mesh tube, is then placed to support the artery walls and keep the blood vessel open. However, in this patient no stent was required because the blockage opened immediately and easily with the balloon dilation, said Parker.
As with the majority of these cases, the patient was awake during the procedure and had local anesthesia in her groin area, where a small incision to insert the catheter was made. “The patient was also kept awake so we could monitor the function of her brain during the procedure and if any stroke-like symptoms were detected, then immediate intervention could be made,” Powell said.
The patient spent one night in PCMH for observation and returned to her normal activities at home within days.
“We determined that carotid angioplasty was the best technique to treat this patient”s carotid artery disease,” Parker said. “In this patient’s case, her rare form of blockage, called fibromuscular dysplasia, which is congenital, is ideally suited to the angioplasty procedure.”
Fibromuscular dyplasia is different from atherosclerosis, or hardening of the arteries, that is the most common cause of carotid artery blockage. Ongoing research at a variety of medical centers throughout the United States and Europe is investigating whether angioplasty and stenting can replace traditional surgery for the more common atherosclerotic carotid blockages. So far the centers report a low risk of stroke during the procedure, Powell said.
Like Powell and Parker, Chiang believes ”that endarterectomy is still considered the gold standard (to treat carotid artery stenosis).