SAFER SURGERY
ECU studies show ways to predict, prevent fibrillation following surgery
Researchers at the Brody School of Medicine at ECU have locked in on an enzyme they think will help tell which patients are likely to suffer atrial fibrillation following mitral valve surgery, cardiac bypass surgery or both. In a related study, they have shown that prescribing concentrated fish oil supplements before the surgery might decrease activity of this enzyme and boost several beneficial properties in the heart, potentially decreasing incidence of postoperative atrial fibrillation.
The discovery could help reduce complications that include stroke, reduce the length of time patients spend in the hospital following surgery and reduce treatment costs.

The enzyme research, “Monoamine Oxidase is a Major Determinant of Redox Balance in Human Atrial Myocardium and is Associated with Postoperative Atrial Fibrillation,” is published in the March issue of the Journal of the American Heart Association. It was funded by a $400,000 grant from the National Institutes of Health.
The study that looked at treating patients with fish oil prior to surgery was published online March 5 in the journal Antioxidants & Redox Signaling. It was funded by the NIH and a $160,000 grant from GlaxoSmithKline, the maker of Lovaza, a prescription-strength fish oil supplement. The pharmaceutical firm also supplied the fish oil capsules for patients.
In the enzyme study, scientists examined human heart tissue samples obtained from approximately 250 patients during heart surgery from 2010 to 2012.
“What we found is that the enzyme responsible for metabolizing epinephrine and dopamine, monoamine oxidase, is a strong predictor of whether a person will have atrial fibrillation after heart surgery,” said Dr. Ethan Anderson, a scientist and assistant professor of pharmacology at the Brody School of Medicine and primary investigator on the study. “In other words, we believe we have discovered enzymes that will predict, with very high degree of certainty, whether a patient is at risk of developing A-fib.”
Once researchers identified patients likely to develop fibrillation, the companion study investigated the impact of prescribing relatively high doses of fish oil to them for two-to-three weeks before surgery. They found the fish oil triggered increased production of key anti-inflammatory and antioxidant enzymes, which helped protect them from post-surgery complications including atrial fibrillation.
“If we have a way of identifying high-risk patients, we can get in front of it,” Anderson said. “Preventing this in the first place would mean they’d have decreased postoperative stay in the hospital, have less complications and less cost.”
“Post-op atrial fibrillation continues to be one of the biggest if not the biggest post op complication for patients undergoing open heart surgery,” said Dr. Alan Kypson, a cardiothoracic surgeon at the East Carolina Heart Institute at ECU. “It accounts for an average of at least two days extra in the hospital, costing about $6 billion worldwide.”
Anderson added that the research could be a springboard to establishing other enzymes as risk predictors for various cardiovascular diseases.
Kypson was co-primary investigator on the enzyme research. Dr. Jimmy Efird, director of epidemiology research at the heart institute and professor of public health, performed the statistical analysis of the project. Graduate student Timothy Darden performed much of the work in Anderson’s laboratory. Dr. Saame Raza Shaikh, assistant professor of biochemistry and molecular biology at ECU, was a member of the research team for the fish oil study, and his laboratory performed the experiments looking at the fish oil in the heart tissue.
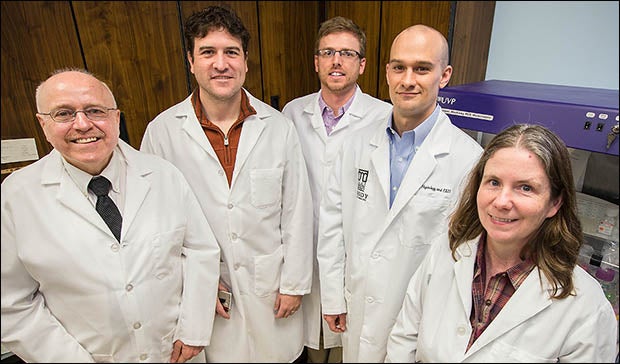
Researchers involved in the study included, from left, Jimmy Efird, Ethan Anderson, Timothy Darden, Stephen Davies and Kathleen Thayne.