Latest therapies for brain cancer now offered in Greenville
Several Greenville health care providers are teaming up to provide state-of-the-art radiation and chemotherapy options for people with brain tumors.
Neurosurgeons from Eastern Neurosurgical and Spine Associates are working with radiation oncologists from the Brody School of Medicine at East Carolina University and Carolina Radiation Medicine to begin offering the GliaSite Radiation Therapy System soon. It delivers radiation directly to the site of the tumor from within the tumor cavity.
The neurosurgeons are also using the Gliadel wafer, which is the first new treatment to be approved for brain cancer in more than two decades. Its manufacturer describes it as the first technology capable of delivering chemotherapy directly to the site of a tumor.
“GliaSite represents a new treatment for patients with recurrent brain tumors who have very few options left,” said Dr. Stuart Lee, a neurosurgeon with Eastern Neurosurgical and Spine Associates. “GliaSite enables patients with recurrent malignant brain tumors to now receive additional radiation, which previously had not been an option for many of them. Additionally, treatment with GliaSite can also be used in combination with surgery when treating newly diagnosed and metastatic brain tumors.”
In addition to Lee, other neurosurgeons at Eastern Neurosurgical who will be using the GliaSite and Gliadel systems are Drs. Douglas Jones, Barbara Lazio and Keith Tucci.
Other local physicians who will be participating in the new GliaSite procedure are radiation oncologists Gordon Koltis of Carolina Radiation Medicine and Ron Allison, chairman of the ECU Department of Radiation Oncology. The GliaSite procedures will be performed at Pitt County Memorial Hospital.
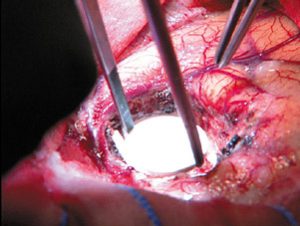
GliaSite works like this: After surgery to remove a tumor, a surgeon places the GliaSite balloon catheter in the space left by the removal of the tumor. The other end of the catheter extends outside the skull and is concealed underneath the scalp. Once the patient has recovered from the surgery, usually three or so days, a solution containing Iotrex, a liquid radiation source, is injected into the catheter and fills the balloon. Iotrex delivers radiation to the edges of the tumor cavity, targeting places where cancer may remain. The patient stays in the hospital three to seven more days, until the right amount of radiation is delivered to the former tumor site. The Iotrex mixture is then withdrawn and the catheter removed during a brief surgical procedure.
In a multi-center clinical trial sponsored by the National Cancer Institute, 21 patients received the GliaSite treatment. They had an average survival rate of 397 days, with a 52 percent survival rate after a year. The system was approved by the Food and Drug Administration last year.
While GliaSite attacks brain tumor cells using radiation, the Gliadel system uses wafers to deliver the cancer chemotherapy drug, carmustine, directly to the tumor site. The therapy is added to surgery to prolong the survival of patients with recurrent glioblastoma multiforme, or GBM, a rapidly progressive and terminal cancer.
After the neurosurgeon removes the brain tumor, he places up to eight Gliadel wafers in the cavity where the tumor was. The wafers slowly dissolve over a period of weeks, delivering the chemotherapy drug directly to the tumor site in high concentrations. By providing localized delivery of chemotherapy, the Gliadel wafers complement other traditional brain cancer therapies while minimizing the side effects often associated with chemotherapy drugs. Unlike chemotherapy taken intravenous or orally which must cross the blood-brain barrier, Gliadel delivers the drug directly to the tumor site.