Health Care Outreach
Like many health professionals who treated patients during the COVID-19 pandemic, Drs. Paul Bolin and Paul Shackleford started to draw conclusions about who was most at risk of dying from infections: people with eastern North Carolina’s typical comorbidities like hypertension, diabetes and obesity.

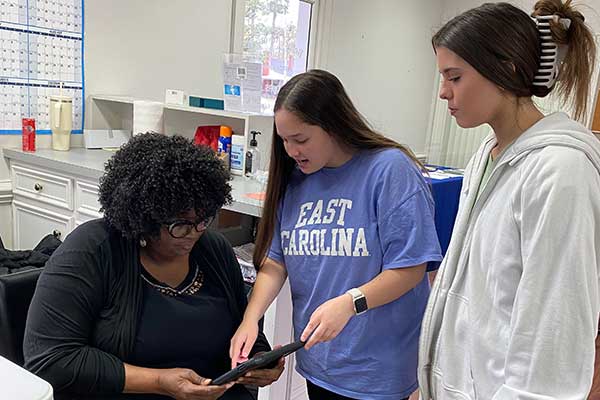
ECU faculty members Drs. Linda and Paul Bolin speak with an employee about the results of a health screening at the Moen factory in New Bern as part of the SERVIRE research outreach project Feb. 1.
Shackleford, a primary care provider and research professor at the Brody School of Medicine, said large swaths of the population served by the heath care structure in eastern North Carolina can be identified through electronic medical records. But that is just part of the equation, leaving a sizable percentage of citizens outside of public health surveillance.
“We started having people novel to our system who were coming into the hospitals, which gave us the idea that maybe we should start looking for people to figure out a mitigation strategy,” Shackleford said.
At the height of the pandemic, Shackleford and a team of health care professionals — Bolin, a fellow Brody professor and chairman of the department of internal medicine, and Dr. Linda Bolin, an associate professor of nursing science in the College of Nursing with expertise in hypertension, and Dr. Ashley Burch, an assistant professor and behavioral health scientist in the College of Allied Health Sciences — were getting requests from businesses across the region to help find ways to keep workplaces functioning and employees safe on the job.
“I don’t have any industrial hygiene or occupational health credentials, but when somebody calls, we have to help” Shackleford said. “One business owner called from his hospital bed recovering from COVID. His business was identified as critical infrastructure, so they were up and running, or trying to run, and struggling because they had employees who were out of work.”
Shackleford said they “didn’t do anything magical” besides reiterating the established guidelines. But having direct contact with workers who likely weren’t getting routine medical care and under public health surveillance spurred Shackleford and the Bolins to consider how they could be proactive in finding citizens with chronic illnesses. The COVID-19 pandemic would eventually subside, but the unhealthiness of rural Southern lifestyles was here to stay. How could they be part of stemming the tide of disease caused by diet and lifestyle choices?
The team inaugurated the SERVIRE (Stopping Early Reversible Vital organ damage In Rural Eastern North Carolina) project and decided that incorporating students into outreach efforts would fulfill ECU’s motto, and overarching mission, of service.

Michael D. Brown, a Moen employee, speaks with research team member Brooke Rose about providing a test sample during a SERVIRE research outreach screening Feb. 1.
To date the SERVIRE project has worked with more than 35 businesses across eastern North Carolina, having engaged nearly 1,400 workers at job sites ranging from a water faucet manufacturer in New Bern to a metal fabrication shop in Ahoskie and a commercial fishing fleet on Hatteras Island.
Researchers initially envisioned more interaction with farm workers, but enough of the potential study participants were undocumented, and reticent to participate, that study directors refocused their efforts to more traditional manufacturing businesses. While they were able to reduce operating cost and complexity, and deal with the privacy issues, the question of why 20-25% of workers flatly refused to be part of the study shifted the focus of the team’s research.
“We have folks that know how to run focus groups sit down and actually ask them, ‘What’s the problem?’” Shackleford said. “Early on in COVID we pivoted to delivering vaccines to individuals who would not go to mass vaccination sites, and it was a similar cohort. Yet they were welcoming of the one-offs that we were able to offer. We didn’t do a lot of vaccines, but we still got in the door.”
Hesitancy would be a continuing challenge, Shackleford knew, but it was better in his mind to achieve what could be achieved to keep small towns in the region from folding.
The Bolins and Shackleford recognize that providing health care to rural communities relies on vibrant and resilient businesses that support the functioning of small, rural communities. Without well-paying jobs, hospitals and community clinics run the risk of losing resources or shuttering altogether.
“If we can keep industry running, we can keep this community fed,” Shackleford said.
Reaching Underserved Communities
For Dr. Linda Bolin, who has advocated for heart health for many years, educating patients on health-promoting lifestyle changes wherever she can is important.
“Some companies, like Moen, want us back all the time, and it gives us an opportunity to talk to them and ask, ‘Well, what changes have you made?’” Bolin said. “It heightens their awareness to know we are going to come back. Sometimes you have to hear things more than once, like with students, you have to repeat it several times for the idea to click.”
Bolin said diet and movement are a huge part of the problem for eastern North Carolina. People who seem relatively healthy because their young bodies can mask systemic health issues might actually be ticking time bombs, health-wise.

Dr. Paul Bolin discusses blood sugar readings with Michael D. Brown, a Moen employee, during a SERVIRE research outreach screening Feb. 1.
“During the Vietnam War we had 18-year-olds dying, and when autopsies were done, they were already suffering from atherosclerosis. Establishing healthy habits and making behavioral changes early in life, before age 20 is crucial,” Bolin said. She stressed that the workforce is often seemingly young and robust but shows signs of unhealthiness from eating fast food and being too exhausted from a 12-hour shift in a manufacturing facility to want to exercise.
“These conditions can take a toll on the body, especially for those with a family history of cardiovascular disease, leading to the onset of pre-hypertension,” Bolin said. “We see a significant number of people with hypertension who are already taking maximum medication doses, leading to a classification of resistant hypertension.”
Bolin likened this situation to developing tolerance to antibiotics after prolonged use — if individuals with resistant hypertension develop severe infections such as sepsis, standard antibiotic treatments may become less effective.
Meloney Quay, a Moen employee from New Bern, said she values the SEVIRE outreach because it’s hard to get in to see a primary care doctor and she usually only seeks medical care in emergencies. She would like to see a clinic at her job site twice a year to keep tabs on her basic health information.
Sapphire LaCoss, who also works on the Moen manufacturing line, said she first participated in the SERVIRE research project because it helped lower the cost of her health insurance. Because both her mother and grandmother are diabetic, she feels a responsibility to keep on top of testing.
“I have four kids. I play football, soccer, basketball and volleyball. I help cheerleading. I like to stay healthy,” LaCoss said. “[The Moen leadership] realizes that we work from 5:30 until almost 4 every day and we don’t have time to go to the doctor, right? I think it’s important that they think that their employees are taken care of and they’ll help us because it keeps us healthy and keeps the business going.”
Brooke Rose runs Rural Carolina Ambulance Service with her husband in Ahoskie and is contracted to do the testing for the research project. She said she gets a lot of satisfaction from helping to identify workers’ health concerns.
“We’ve caught very high blood pressure or that they are diabetic and didn’t know they had it. Then they can get the help that they need,” Rose said. “We’ve seen them later and their levels were down, their blood pressure is better and they’re very appreciative. They’re grateful.”
Teaching Students
SERVIRE is formally a research project, working to establish best practices for how to identify workers who have fallen through the cracks of the health care system. But the project leaders have turned it into a teaching opportunity — students and contracted medical workers assess workers for basic health metrics that can identify precursors for serious medical complications: height and weight, body index, neck circumference and basic blood sugar readings.
ECU Honors College students Sarah Elliott, a nutrition major, and Paige Brown, a biology major, take measurements of an employee as part of a SERVIRE research outreach project at a call center in Greenville. (Contributed photo)
The research is important for the immediate health of the individuals who are tested, and the study directors hope their work will impact regional health in the long-term, but the outreach efforts also give ECU students hands-on experience working with the high-risk populations they will serve after graduation.
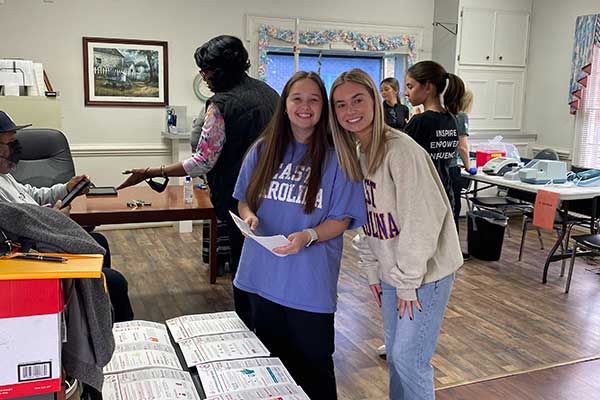
Linda Bolin and Burch offer an Honors College seminar for pre-nursing and health majors that focuses on chronic diseases in eastern North Carolina and provides students with the opportunity to participate in the SERVIRE project.
Their seminar, titled “Ghosting Premature Death: Promoting Prevention in Eastern North Carolina,” emphasizes the importance of early engagement with health-related majors by exposing potential students to population health issues and social determinants of health.
“Having these students, along with pre-medical and pre-nursing students, volunteer as integral members of the team is essential because it recognizes the significance of investing in future doctors, nurses and other health care workers, instilling in them a sense of service to their community,” Linda Bolin said.
Several students who were enrolled in the Honors College seminar as pre-nursing majors are now first semester students in the College of Nursing.
Kaylee Ontiveros, an Honors College nursing student from Ayden, said it was eye-opening for her to see just how far from primary care options many of the workers were, and how having hands-on experience with patients can tie together book learning and classroom lectures.
ECU Honors College students Sydney Faulk, a public health major, and Paige Brown, a biology major, take measurements in a SERVIRE research outreach project at a call center in Greenville. (Contributed photo)
“A lot of people struggle to get medication or get to the hospital compared to places like our city, where can get to doctors right down the road,” Ontiveros said. “We saw a patient who had an abnormality in her neck that she didn’t know about. We said, ‘OK, you need to check this out,’ so it was really putting everything from classroom into perspective.”
Gracyn Faulk, a fellow Honors College nursing student from Goldsboro, participated in research visits to a call center in Greenville and a soup kitchen. She agrees that having an opportunity to interact with real patients was a benefit to her education.
“It’s not what I expected. I’m not really sure what I expected. But it was good to see some of the social determinants of health that we talk about in class, to see them in real life. Some of the people had stories that you wouldn’t hear otherwise,” Faulk said.
Gracie Ipock, a first semester Honors College nursing student from Morehead City, was with Faulk. She said being in the community and learning about people was a huge benefit. Ipock had previously worked as a certified nursing assistant, but this was a new way to interact with patients.
“I think it will help me to be better at clinicals like now because I’m able to talk to these people and not be so scared,” Ipock said. “The more confident you are with working with them, the more they’re going to feel relaxed. Someone could look perfectly fine and not know that they have a lot of issues going on with their health.”
