Rural Health Symposium highlights equity, oral health, COVID-19 impact
Health equity, oral health, resilience and the impact of COVID-19 on rural health care were some of many topics covered at the fifth annual Rural Health Symposium on Feb. 23-25.

Participants in the Rural Health Symposium at Eastern AHEC took part in a poverty simulation to better understand the challenges facing those who live in poverty. (Photos by Cliff Hollis)
Around 140 people participated in the conference both virtually and in person at Eastern Area Health Education Center, which hosted the conference along with the Brody School of Medicine at East Carolina University, ECU Medical & Health Sciences Foundation, Vidant Health, and Triangle Healthcare Executives’ Forum of NC (THEF).
“This was Eastern AHEC’s first hybrid offering of this size and our rural participants appreciated the virtual option to reduce the financial barriers associated with attending,” said Mary Stuart Peaks, MPH, CHES, assistant director, Continuing Medical, Dental and Pharmacy Education at Eastern AHEC. “Thanks to our partners, such as the Medical & Health Sciences Foundation, we were able to keep registration costs low as well for this critical educational event.”
The multidisciplinary symposium allowed healthcare professionals and community leaders from across eastern North Carolina to come together to share innovative and collaborative efforts to provide better care to areas with limited resources.
“There’s the stereotype of rural areas as white and older and agricultural, but there’s a lot more diversity in these areas,” said Dr. Gbenga Ajilore, senior advisor, Office of the Under Secretary for Rural Development, U.S. Department of Agriculture, in his virtual presentation. “At first, we thought COVID-19 wouldn’t impact rural areas with sparse populations, but we were wrong — dead wrong. There are impacts we’re still feeling to this day. There are huge disparities depending on if you’re in a metro or non-metro area. But it isn’t about what these rural areas don’t have. Diversity is the strength of this country, of these communities.”
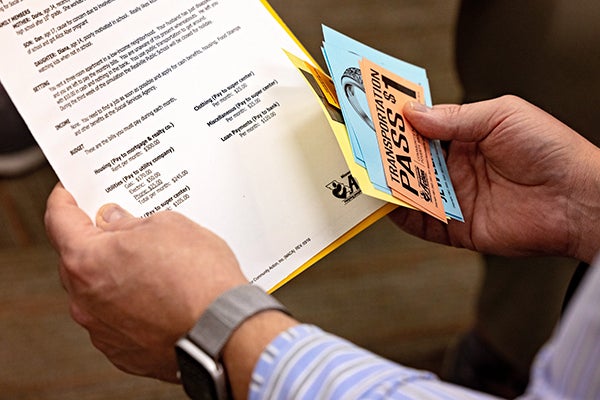
The poverty simulation activity at the Rural Health Symposium gave each participant a simulated life and budget to manage to better understand how those in poverty work through challenges every day.
In addition, Dr. Paul Bolin, Jr. and Dr. John M. Diamond shared their outlook on “long COVID” or “chronic COVID” — correctly called PACS or Post-Acute COVID Syndromes – in both adults and children.
An interactive poverty simulation led by the Department of Health Education and Promotion in the College of Health and Human Performance at ECU helped in-person participants understand the difficulties of navigating life with limited resources. Meanwhile virtual participants heard sessions on lifestyle medicine, which focuses on preventing rather than treating disease.
“Poverty is not a game for the 37.2 million US citizens living in poverty (as of 2020) whose lifestyles you will simulate,” organizers said. “You are going to try to walk a mile in the shoes of those who are poor. The money is pretend, but the statistics are real.”
An Innovations Panel showcased how communities in eastern North Carolina are addressing the Healthy NC 2030 priorities to improve health equity, such as life expectancy, health literacy, access to healthy food, primary care workforce, and more. After an open call for submissions, eight projects were selected:
- Life Expectancy — The Health Hazards of Climate Change: A Study on Extreme Heat and Dehydration among Farmworkers in Eastern North Carolina
- Health Literacy — Augmenting Rural Patient Health Literacy with Videos for Cancer Patients
- Health Literacy — Vaccine to Farm Project: A Healthcare System Supporting Vaccine Efforts to the Agricultural Communities of Central NC
- Uninsured — Rural Patient Navigation: Addressing Barriers to Quality Cancer Care
- Access to Healthy Food — More PEAS Please! A Multidisciplinary Approach to Improving Dietary Quality, Cognition, and Language Among Low-Resource, Racial/Ethnic Minority Preschool Children (3-5 years) at FEED (Food-based Early Education Lab).
- Life Expectancy — Partnering with Employers in Eastern North Carolina to Provide Worksite-based Health Assessments in Rural Communities
- Primary Care Clinicians — Roanoke Chowan Community Health Center Medical Assistant Workforce Development Program
- Suicide Rate — Enhancing Access, Quality, and Outcomes of Mental Health Care in Emergency Departments: Expansion of the NC Statewide Telepsychiatry Program (NC-STeP)
Another panel discussed the importance of connecting oral health to whole body health. Panelists described how training dental and medical students together and sharing resources can help bridge this gap.
“The oral-medical divide is not just a dental issue,” said Dr. T. Robert Tempel Jr, associate dean for extramural clinical practices at the ECU School of Dental Medicine. “It’s something facing our whole nation, and in North Carolina, our work can make a difference.”
Guest speakers from Womack Army Medical Center, Naval Medical Center Camp Lejeune and Vidant Medical Center shared how they are cultivating resilience among their personnel for the benefit of healthcare professionals across the region.
The physical and mental health of farmers and other agricultural workers were also highlighted. In North Carolina, there are around 1,400 disabling injuries and 20 deaths per year from tractors and other equipment. Nationally, farmer and rancher suicide rates are noted to be 3.5 times that of the general population. Speakers emphasized the need for practitioners to be aware of these risk factors.
For more information on upcoming continuing education programs at Eastern AHEC, visit www.easternahec.net.