PARKINSON’S DISEASE SURVEY
ECU researchers identifying needs of individuals with Parkinson’s disease in the East
East Carolina University researchers are hoping to understand which resources are available to those with Parkinson’s disease (PD) in eastern North Carolina, how they are being utilized, and what types of services are most needed.
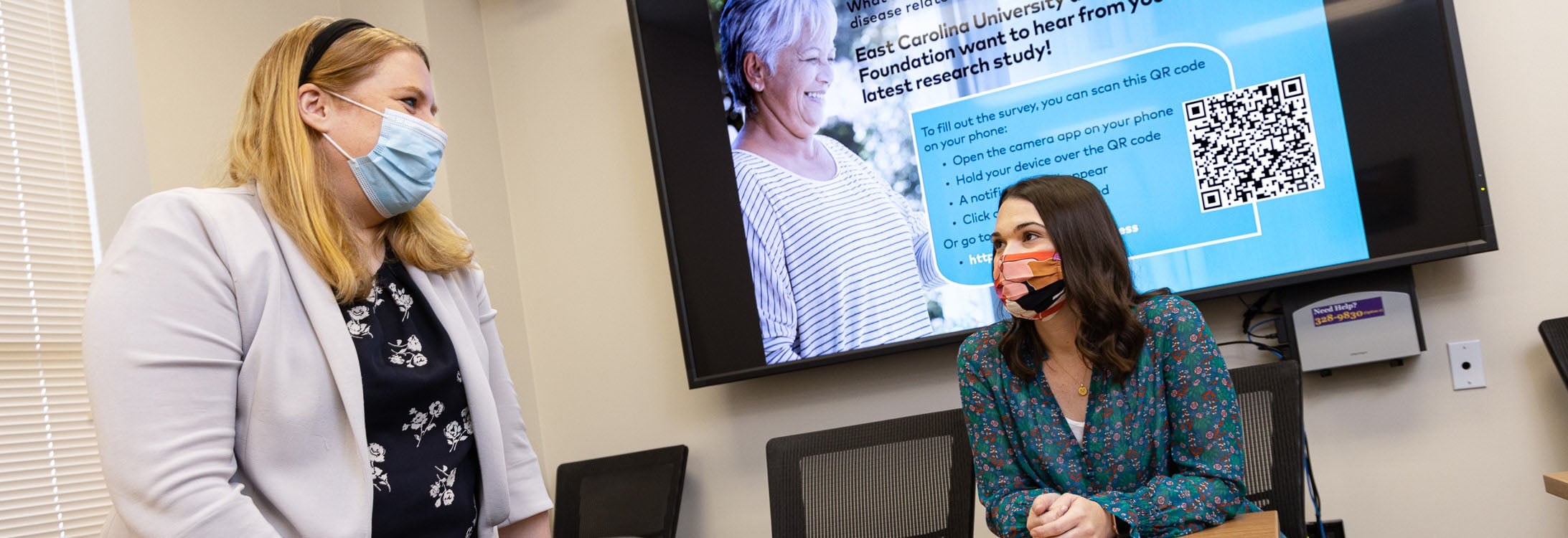
ECU College of Allied Health Sciences faculty members Dr. Kathrin Rothermich and Dr. Lauren Turbeville, along with cross-campus collaborator Dr. Jennifer Hodgson (Department of Human Development and Family Science), local individuals with Parkinson’s, and support from The Parkinson’s Foundation, are conducting a survey for individuals in eastern North Carolina with Parkinson’s disease.
They hope that with more precise data on the challenges that eastern North Carolinians with Parkinson’s face, they’ll be better positioned to lobby for those resources.
“This is really about how we can help them now with resources,” said Rothermich, an assistant professor in the Department of Communication Sciences and Disorders. “To do that, we really need to know what’s needed, what’s a priority, and what the biggest concerns are.”
Parkinson’s Disease (PD) is a neurodegenerative brain disorder that leads to uncontrollable movements, stiffness and difficulty with everyday activities like walking, balance, cognition, swallowing and speaking. It is challenging to diagnose and there is currently no known cure.
Data from the survey will assist researchers in understanding where the needs are greatest and aid in lobbying for more resources for those with Parkinson’s Disease (PD) in eastern North Carolina.
Approximately 60,000 people in the U.S. are diagnosed each year, and nearly 1 million people nationwide are living with PD, according to the Parkinson’s Foundation. But for those patients living in eastern North Carolina and other rural areas, the specialist treatment they need can be difficult to access, which also results in a lack of awareness about the other resources available to them.
“There’s not much east of Raleigh for people with PD in terms of a movement disorder specialist,” said Turbeville, an occupational therapist and assistant professor in the College of Allied Health Sciences’ Department of Occupational Therapy. “That’s typically who diagnoses and ideally treats them.”
Turbeville has witnessed first-hand the struggles that those with Parkinson’s often face in accessing the care they need — particularly when they live in rural areas.
“My dad has Parkinson’s and my granddad had Parkinson’s,” she said. “My dad lives in South Carolina and has someone drive him three hours to Charleston to see a movement disorder specialist once every six months. He’s lucky because he has me and I’m an OT, but other people don’t have that luxury and are missing out on a lot of opportunities for other specialties.”
Similarly, because there are no movement disorder specialists in the eastern part of North Carolina, patients often must find help to make long journeys to those appointments.
There are, however, other allied health professionals in the East trained to help manage a person’s PD symptoms — including physical therapists, occupational therapists and speech-language pathologists. Because patients lack a go-to specialist or center in the region, they’re not always aware of these resources available to them that are often covered by their insurance, and it’s difficult to track whether PD patients are able to access the other resources they need.
Rothermich and Turbeville hope that their survey — which they said should take about 10-15 minutes to complete — will lead to those answers and guide their next steps toward lobbying for the most needed resources.
“PD is certainly not the only disease where people struggle finding care in this region, just because it’s so spread out, and also there’s a lot of socioeconomic insecurities and health literacy issues. All of these things come into play,” Rothermich said. “I think there are some communities we’re just not reaching right now, especially marginalized minorities that are not currently connected to PD support groups.”
“Regional transformation is at the heart of ECU’s mission,” College of Allied Health Sciences Dean Dr. Robert Orlikoff said. “Our focus on diagnosis, treatment, care and rehabilitation for the underserved helps empower individuals, families, and communities in the East lead better lives with more options and opportunities. Access to quality interprofessional health care, such as needed by those with Parkinson’s, will be key to this important effort.”
As ECU and Vidant Health partner to create ECU Health in an effort to provide more comprehensive care and better service throughout the East, Rothermich and Turbeville think the time is right to explore these questions in more detail.
“ECU Health will be a national model for academic rural health care and will pave the way for unique opportunities to quickly translate this kind of important research into improved health care delivery to those in need,” said Dr. Michael Waldrum, dean of ECU’s Brody School of Medicine and CEO of Vidant Health. “This shared focus on tackling the complex health care challenges of eastern North Carolina will better enable us to identify, address and advocate for the health needs of all residents in the East.”
If you’d like more information about this research, visit the Social Communication and Neuroscience Lab website online. If you’re interested in helping or getting involved with this initiative, please contact Dr. Kathrin Rothermich (rothermichk17@ecu.edu) or Dr. Lauren Turbeville (turbevillel20@ecu.edu).