RURAL HEALTH
Better health outcomes for rural North Carolinians focus of annual symposium
During the 4th annual Rural Health Symposium, health care providers tuned in for a live webinar to share ideas that could translate to better health outcomes for rural patients.
The annual event, sponsored by Eastern AHEC, offered interprofessional sessions, panels and presentations that focus on collaborative efforts to provide better access to health care for rural North Carolinians.
The event was also sponsored by the Office of Continuing Medical Education of the Brody School of Medicine at East Carolina University, ECU Medical & Health Sciences Foundation, ECU Department of Public Health and the Triangle Healthcare Executives’ Forum of North Carolina.
The panel discussions and breakout sessions featured a variety of health care providers and students in medicine and public health, who shared insights and experiences for treating patients in the field—before and during the COVID-19 pandemic.
Before kicking off the day’s events on Thursday, Feb. 25, Dr. Lorrie Basnight, executive director of Eastern AHEC and associate dean for continuing medical education at Brody, welcomed participants and shared the vision of the event as “the idea of a symposium that would cross all health professions” and bring people together to assess the region’s unique health challenges.

During the Rural Health Symposium Feb. 25, Kay Craven, ECU Physicians nutrition and patient education section head, outlined programs for patients that had shifted to online and other innovative methods, such as a drive-through grocery pick-up for a healthy living class. (Photo by Rob Spahr)
During the session, “NC Crossing Boundaries Together,” speakers highlighted the potential across North Carolina for a collaborative approach to health care. Maggie Sauer of the N.C. Department of Health and Human Services Office of Rural Health and Patrick Woodie of the N.C. Rural Center discussed keeping an eye to the future for opportunities to launch partnerships.
“It’s important to not just think about what we’re doing right now,” Sauer said. “I know we’re going to talk about continuing the great work we have in North Carolina.”
They encouraged participants to look for solutions beyond what they think is attainable.
“All of us think about crossing boundaries and not being siloed in our work,” Woodie said, adding that health care providers should keep in mind the characteristics of rural North Carolinians including the challenges that factor into pursuing health care.
Before the pandemic, Woodie said, about 600,000 North Carolinians were without health care coverage. That number has jumped to nearly 1.2 million in the wake of job losses and other factors spurred by the pandemic.
Community health workers have helped ease the burdens on rural health care providers through training, earning the trust of communities and working to link resources with the people who need them. That system is an example of what can come from partnerships among state and community agencies as well as providers.
Woodie emphasized the need for broadband in rural communities for telehealth connections and for a network of leaders and partners that facilitate collaborative work toward health for rural areas.
During the COVID-19 Innovations Session, presenters explained how their programs, offices and agencies pivoted during the pandemic to meet constituents’ needs in new ways.
Anna Beth Robertson, a medical student at Brody, talked about her work with the Greenville Community Shelter Clinic, which had limited patient care options pandemic set in. Robertson said telehealth visits were the key to keeping the clinic running and caring for homeless patients—a vulnerable population particularly susceptible to chronic conditions.
With the help of community and ECU partners, telehealth was able to see patients and prescribe much-needed medications.
“We really needed to be able to talk to our patients in order to get them the best care possible,” she said. “We really engaged being able to meet our patients where they are and see them face to face.”
Shantell Cheek of Access East and Vidant Health talked about working to ensure that farmworkers had access to information on COVID-19 and how to protect themselves—enlisting bilingual employees to help ease communication and transportation barriers in the process.
Among other speakers, Kay Craven, director of nutrition services at ECU Physicians, gave an overview of how programming geared toward nutrition education shifted online when the pandemic hit, resulting in creative solutions like a drive-through grocery pick-up for program participants to use for healthy recipes.
ECU nutrition sciences student Brandon Stroud outlined the benefits of a “produce prescription” program that partners with local clinics and other partners to provide fresh produce to patients living with chronic illnesses.
Other symposium topics included climate equity, agromedicine, dementia and rural living, health advocacy and stress and anxiety during COVID-19.
During the Feb. 26 breakout session, “Dentistry in Remote Locations: Lessons from the Armed Forces,” dentists serving in the U.S. Armed Forces outlined how their experiences and resources could translate to better access to dental care for rural North Carolinians.
The session’s speakers included Army Maj. Gamal Baker, a comprehensive dentist at Fort Bragg; Navy Lt. Cmdr. Megan R. Carter and Air Force Maj. John R. Mallya, both in their services’ Dental Corps as well. The discussion was facilitated by Dr. T. Rob Tempel, associate dean for extramural clinical practices for the East Carolina University School of Dental Medicine.
Baker highlighted the Army’s efforts to transform dental care through technology and access in remote locations and a variety of situations—and the importance of having fast and mobile resources that mimic dental office set-ups as closely as possible.
“We’re trying our absolute best to bring that fixed facility standard to the field,” he said.
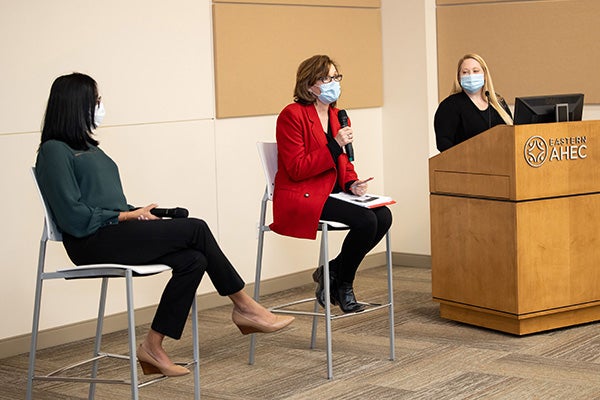
Dr. Anokhi Patel, left, Fellow in the Division of Hematology/Oncology in the Brody School of Medicine, and Kay Craven, center, ECU Physicians nutrition and patient education section head, participate in the Rural Health Care Symposium at Eastern AHEC as Mary Stuart Peaks of Eastern AHEC facilitates. (Photo by Rhett Butler)
Carter described a routine dental office on a Navy ship, stressing that most dental areas on ships are not equipped to treat civilians during humanitarian missions or disasters but can set up in alternate sites to meet needs in those situations. The offices instead focus on routine and as-needed care for sailors.
Navy dentists, she added, also focus on providing care to units “while they’re home and get them ready to deploy.”
Mallya, a comprehensive dentist at Seymour Johnson Air Force Base, said the theme in any situation is “readiness.”
“The key theme,” he said, “is that readiness is always the central focus with our mission.”
The innovative readiness training Mallya described could help dentists in rural areas adapt to the resources they have available, assess situations and reach out to other professionals for additional input.
All three speakers emphasized the opportunities that exist in the advancement of teledentistry— the use of information technology and telecommunications for dental care, consultation and education.
“Teledentistry is still a relatively new concept for the Air Force,” Mallya said, “but we’re excited to see what capabilities are in the future.”
All three also voiced optimism in overcoming challenges like connectivity issues or time zone differences that can hinder teledentistry consultations in real time. When the processes come together, however, the results can improve patient outcomes and make dentists feel less isolated in the field by making experts accessible through technology.
“Knowing you can provide that level of care, even when you’re out in the ocean, is very comforting,” Carter said.
Tempel said rural dentists can feel isolated as well, a problem that the ECU dental school’s teledentistry network on campus and at its community service learning centers across the state are working to address—in part through collaborations with community and state partners.
“The teamwork you’ve talked about really needs to exist in civilian dentistry,” he said. “Through teledentistry, that can happen. We all have the common goal of improving health in North Carolina.”
