FUNDING COVID-19 RESEARCH
How ECU’s Brody School of Medicine will use $15M in CARES Act funding
East Carolina University’s Brody School of Medicine will put the CARES Act funding it received from the North Carolina General Assembly toward developing better treatments, advancing vaccine research and minimizing COVID-19’s impact in the region and state while contributing to the global body of knowledge about the novel coronavirus.
More than 20 different projects have received funding from the $15 million the school was granted by the state legislature for COVID-19 initiatives. The projects primarily fall into three categories related to COVID-19: treatments to enhance innate immunity to the virus, vaccine development and community testing initiatives. Other funded projects aim to support high-risk and rural populations in the region and advance efforts to slow transmission.
Several projects receiving funding will benefit from two newly renovated Biosafety Level 3 laboratories (BSL3) which are outfitted according to governmental guidelines to allow scientists to safely study infectious agents or toxins, such as SARS-CoV-2, the virus that causes COVID-19, that can be transmitted through the air. These lab upgrades include upgraded airflow, filtration, improved seals to doors, animal housing, sterilization and enhanced security. Other funds will allow the Department of Anatomy and Cell Biology to purchase new equipment to process and evaluate tissue samples infected with pathogens such as SARS-CoV-2. Together, these represent a first-class research facility for conducting research on the disease and will help Brody to conduct research beyond that funded by the CARES Act.
Although the legislature’s funding has been designated for the fight against COVID-19, the collective understanding gleaned from it will continue to provide benefits for years to come.
“If you study cystic fibrosis, you learn a lot about how lungs work,” said Dr. Peter Schmidt, vice dean of the Brody School of Medicine. “We study diseases and it gives us insight into the normal function. COVID-19 is no different.
“We’re going to get a lot of insight into things that we didn’t understand in the human body beyond how to treat this disease. So, we’re going to build out resources to understand COVID, but it’s going to give us insight into work that will continue as we understand other aspects of health.”
Enhancing immunity
Several projects receiving funding from the grant will work toward the development of treatments to prevent and treat infection.
Dr. Paul Bolin is leading the Brody School of Medicine’s research and clinical trials using convalescent plasma to treat COVID-19. More than $1 million from the CARES Act funding will be used to generate additional insight from these studies through clinical trials of some of the therapeutic agents identified from these earlier ECU studies that have shown potential to enhance patients’ immune responses.
“Commercial partners will produce a class of treatment called a clonal antibody from this research,” Schmidt said. “That’s an advance from the kind of a ‘Hail Mary’ approach we’ve been doing to date where we hope these recovered patients have something in their blood that’s going to help to a more targeted treatment.
“ECU has really been central in that progression. We started out just asking anybody who recovered to donate blood and now we’re part of a clinical trial through Dr. Paul Cook which is one of these monoclonal antibodies.”
Another project receiving funds geared toward enhancing immunity is headed by Division of Hematology and Oncology’s Dr. Li Yang, who has done extensive research on the transmembrane receptor GPR4. Yang has evidence that this receptor may be important in modulating individuals’ immune response. Better understanding GPR4’s effects could play a role in helping to reduce COVID patients’ risk of developing acute respiratory distress syndrome, a common, life-threatening complication resulting from the disease. Yang and his team are among those who will work in the new BSL3 labs.
A project led by Dr. Mark Mannie, a faculty member in Brody’s Department of Microbiology and Immunology, received funding that will further his research into “infectious tolerance” — the process of moderating the immune response to infection to limit potentially harmful immune system response. Being able to more safely and reliably control immune system responses such as the cytokine storm often seen in COVID patients would help to reduce morbidity and mortality from the disease.
Meanwhile, faculty in Brody’s Department of Biochemistry have identified three proteins in SARS-CoV-2 to focus on. Directed by department chair Dr. John Cavanagh, Brody’s Dr. Tonya Zeczycki and Richele Thompson will work with other faculty and at least six PhD students looking for ways to inhibit the interaction of these SAR-CoV-2 proteins with their potential host.
The results have implications for treatments and vaccine development.
“We’re trying to figure out how the virus sticks to endothelial cells,” Cavanagh said. “We’re going to map the interface between the two. If you can stop the virus from touching something it’s not supposed to, then it will not infect it.”
The proteins they’ve identified represent key regulatory steps in the virus’ lifecycle from three different areas, Zeczycki said.
“It’s coming at it from different angles, which is good if you have a patient who may not handle one way or another that this will give you options for hitting different targets,” Zeczycki said.
The students jumped at the chance to participate in research that could have an immediate impact on a global scale.
“It’s very rare that you get to do this — about once every 100 years — where you’re actually tackling something that’s going on in real life,” Cavanagh said. “People have cancer and Alzheimer’s, but those seem a bit distant. Whereas, we’re all wearing masks because it’s happening to us all right now. That’s why I think all the students have been so excited to treat something right now.”
“The sense of urgency I think with this is just different,” Zeczycki said, “which brings a new energy to the students and even to us as faculty, you just kind of drop everything and say, ‘This is what we’re focusing on right now.’”
Vaccine development and implementation
ECU has one of the world’s leading microbiologists studying coronaviruses working to develop a vaccine. Dr. Rachel Roper, an associate professor in the Department of Microbiology and Immunology, led the team that first sequenced the SARS-CoV-1 coronavirus. Funding from the legislative appropriation will help support this work as Roper will utilize one of the new BSL3 labs to test immune responses to potential SARS =-CoV-2 vaccines targeting the whole virus using animal models.
“This really allows us to do the vaccine studies,” Roper said of the legislature’s support. “We couldn’t have done it without that funding. This allows us to make the vaccine and test it, and to actually grow the virus. If you can’t grow the virus, there’s a lot of stuff you can’t do. We really need to be able to grow the virus, and challenge the animals, and that’s what the Biosafety Level 3 lab will allow us to do.”
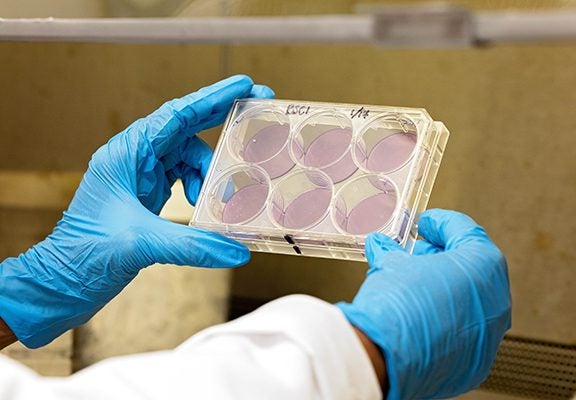
Dr. Rachel Roper observes changes in lab samples created as part of her research. (Photo by Cliff Hollis)
Although other SARS-CoV-2 vaccine candidates have reached advanced stages of testing, they target only a small portion of the virus, which could make them less effective, Roper said.
“Most of the vaccines (that are in advanced stages of development now) are targeting one protein — that’s a very small part of the genome. It’s not a very big target,” Roper said. “Some of the vaccines are only targeting a piece of the protein. That’s not going to give you a strong enough immune response, and I’m worried that that target is too small. If you have a small target, the virus can mutate away from it.”
Roper is also collaborating with the School of Dental Medicine to pilot a saliva-based platform for testing COVID-19 through dental clinics across the state. This research aims to improve testing methods, including evaluating the potential for wearable technology devices and computer algorithms to monitor and predict health and infection risk.
Although mass media have focused heavily on the timeline needed to develop a safe and effective vaccine, less time has been spent discussing the logistics and ethics of implementing a COVID-19 vaccine once one is deemed suitable.
A partnership project between ECU and Vidant Health, led by Dr. Greg Kearney from Brody’s Department of Public Health, along with expert geographers from the Thomas Harriot College of Arts and Sciences and information technology experts in the College of Allied Health Sciences, are working to develop a data driven mapping system to identify and target locations of COVID-19 high-risk, vulnerable populations, hot spots and high priority areas for fast and efficient distribution of vaccine throughout eastern N.C.
Dr. Maria Clay, chair of Brody’s Department of Bioethics, leads a team focused on creating an ethical framework to address questions such as determining when vaccine access should be expanded to include more vulnerable populations who were not included in clinical trials due to the increased risk associated.
Community testing initiatives
A portion of the funds provided from the legislature will allow for more in-depth testing to track different mutations of the virus throughout the region.
Dr. John Fallon, chair of Brody’s Department of Pathology who also serves as the chief of Vidant Medical Center’s hospital laboratory, has become a recognized state leader in COVID testing, completing more than 90,000 RT-PCR tests on more than 72,000 patients through Aug. 28. The money his department received from the legislature will help to expand its capacity to track the virus’ mutations throughout our region and study how genetic factors are linked to clinical outcomes in COVID patients.
A study headed by Dr. Suzanne Lea and Dr. Arron Kipp in the Department of Public Health is assessing the correlation between students’ attitudes and the spread of COVID-19. The project expands upon the Community Testing and COVID-19 Testing Study, ComPACT, which targets recruitment toward rural, diverse and medically underserved individuals in the local community.
In a follow-up study of non-hospitalized SARS-CoV-2-positive patients, Brody medical students are assisting the medical school’s associate dean for research, Dr. S. Russ Price, in conducting follow-up calls with ECU Physicians patients who tested positive for the virus, but whose condition did not warrant hospitalization in order to track symptoms and recovery progress.
Additional projects
Additional projects receiving CARES Act funding focus on supporting high-risk and rural populations throughout the region, improving supply and use of personal protective equipment (PPE), and improving the infrastructure necessary to support other projects’ success.
Diabetes, obesity and stroke are common in eastern North Carolina. Because diabetes and obesity are also significant risk factors for those infected with COVID-19 and insulin can contribute to obesity in type 2 diabetes, Brody’s Nephrology Division within the Department of Internal Medicine is working to convert those type 2 diabetes patients who use insulin to non-insulin therapies. The long-term effects of SARS-CoV-2 infection on patients at high risk of stroke, meanwhile, are unknown. Brody’s Department of Medicine will track these patients at high risk of stroke over time to better understand how these conditions correlate.
More patients in rural areas of eastern North Carolina will have better access to specialized care as a model for telehealth pioneered by Dr. Sy Saeed is expanded to allow all medical specialties and dental medicine to provide care into rural communities.
Dr. Sinan Sousan for the Department of Public Health and the North Carolina Agromedicine Institute leads a team of scientists and physicians working to study face mask effectiveness to produce a prototype respirator with similar efficacy to the gold-standard respirators that are in short supply. Support from the general assembly will also be used to partially fund PPE training for health sciences students, so that they are better able to protect themselves, their environment, and answer questions from patients about PPE use.
“We are so grateful to the state for supporting our work. Eastern North Carolina has a diverse population whose experience of COVID-19 is multifaceted. Across differences in transmission patterns, availability of testing in rural communities, and a population that includes many people with underlying health conditions that puts them at risk of severe disease, the Brody School is well positioned to make an impact locally and draw insight into the disease that can help everyone,” Schmidt said. “Because of the breadth of impact of COVID-19, it is a challenge well-suited for ECU. We need to draw on vision for healthcare that we bring with our integrated Health Science Division in order to address challenges that span public health, medicine, nursing, allied health, and dentistry.”
