STATINS IN FOCUS
Study examines side effects of cholesterol medications
Millions of people in the U.S. take statins, a class of drugs prescribed to lower cholesterol, reducing the risk of heart disease and other health problems. Now, researchers at East Carolina University and the University of Kansas are taking a closer look at one of the side effects of statins in order to better understand the potential impact of daily usage.
Dr. Darrell Neufer, director of the East Carolina Diabetes and Obesity Institute, and Dr. John Thyfault, associate professor of physiology at the University of Kansas Medical Center, have been awarded a five-year, $3 million grant from the National Institutes of Health to evaluate the impact of statins on mitochondrial function in muscle tissue.
Previous studies in mice suggest that statins might negatively impact the function of mitochondria — the parts of cells that break down nutrients to create energy — in muscle, Neufer said. And research published by Thyfault found that patients taking statins while starting an exercise program didn’t see the full benefit of the exercise.

A multi-institutional study is examining the side effects of commonly prescribed cholesterol-lowering drugs known as statins.
“We found that if people took statins while they started an exercise program, they didn’t adapt to the exercise,” Thyfault said. “So the number of mitochondria in their skeletal muscles didn’t increase like they should with exercise, and their overall, whole-body aerobic fitness didn’t increase like it should have.”
Neufer and Thyfault, who were both mentored by Dr. Lynis Dohm at ECU earlier in their careers, decided that a comprehensive study in humans was needed. They conducted a pilot study with patients starting a high-dose statin regimen; biopsies were taken before starting the regimen and at two weeks, one month and two months.
“We measured the mitochondrial capacity to consume oxygen, basically the maximum capacity of the mitochondria,” Neufer said. “To our surprise, the capacity progressively dropped, and it was cut in half within two months of starting the high-dose statin.”
Such a drop in mitochondrial function could have important implications including muscle pain, increased risk for diabetes and decreased response to exercise.
Neufer and Thyfault are careful to note that they don’t want to dissuade people from taking statins.
“Statins have had a tremendous impact on cardiovascular disease prevention,” Neufer said. “But that doesn’t mean that we shouldn’t learn everything we can about the potential effects of statins, so that physicians and patients can be better informed and make better informed decisions.”
Neufer said that patients who have already had a cardiovascular event should certainly be on a daily statin treatment, because it lowers the risk of having another event. But there may be cause for restraint in using them as primary prevention — that is, prescribing them to people who have not had a cardiovascular event but may have elevated risk factors.
“That’s where I think we have to be more careful,” Neufer said. “Because if the drugs make your mitochondria accelerate their aging process, if they make people have muscle pain, make them less physically active and have their aerobic fitness go down, those are important health factors to consider. It really gets down to the risk-benefit ratio.”
The grant-funded project has two objectives. The first is to test the impact of different doses of statins on mitochondrial function and cardiorespiratory fitness (compared to a control group taking a placebo) over one-month, six-month and 12-month periods. The second is to follow up on the interaction between statins and exercise.
“We wondered if you took a low-dose statin and exercise, if you could respond normally,” Thyfault said. “So we’ll have high-dose, low-dose and placebo groups that are going to take those and start exercising. We’ll measure the effects at baseline and at 12 weeks, using the same kind of outcome measures — mitochondrial function and whole-body aerobic fitness.”
The multi-institutional collaboration will provide more subjects and more lab space than either institution would have on its own, as well as increasing the diversity of the population.
Ultimately, said Neufer, “We want to provide physicians with as much information as possible to make the best decisions possible.”
The research will help inform who should and shouldn’t be on statins, at what doses, and improve the medical community’s understanding of the risks and side effects.
If you are between the ages of 35-60 and are potentially interested in participating in the study, please contact Gabe Dubis at dubisg@ecu.edu.

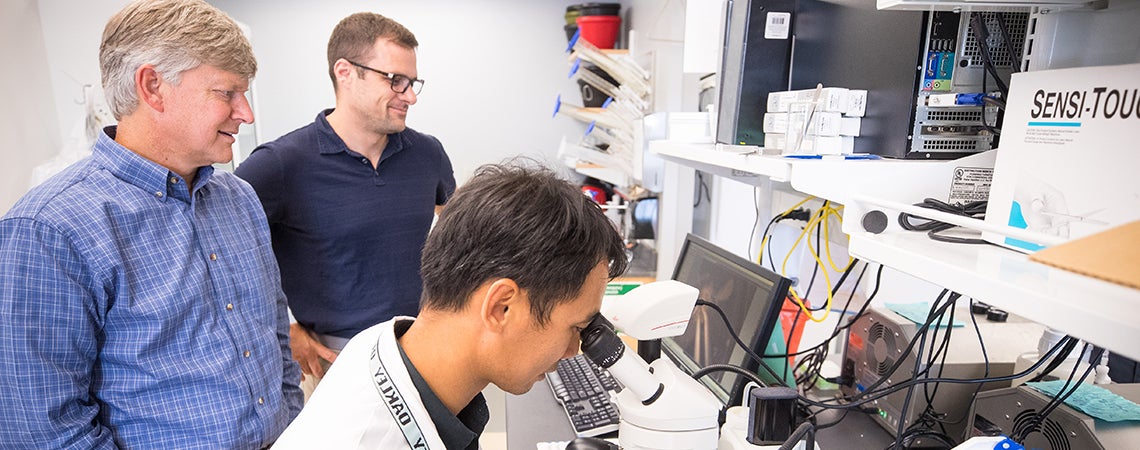
Dr. Chien-Te Lin (left) and Dr. Colin McCoin work out testing procedures to ensure consistency between labs at ECU and Kansas University Medical Center
Reputation for Research
Dr. Lynis Dohm was instrumental in establishing the East Carolina Diabetes and Obesity Institute, along with Dr. Walter Pories and Dr. Joseph Houmard; and Dohn’s students, including Dr. Darrell Neufer and Dr. John Thyfault, have made considerable contributions to the field of mitochondrial biology and metabolism. Neufer was recently invited to Stockholm, Sweden to deliver the David Murdock-Dole Lecture at the annual meeting of the Mayo Clinic-Karolinska Institute Collaborative Research Conference.